About the Conference | Schedule | Conference Locations and Registration | Schedule Long Version (including Abstracts)
Download „About the Conference“ here
Schedule
Download short version (without abstracts) here
Conference Locations and Registration
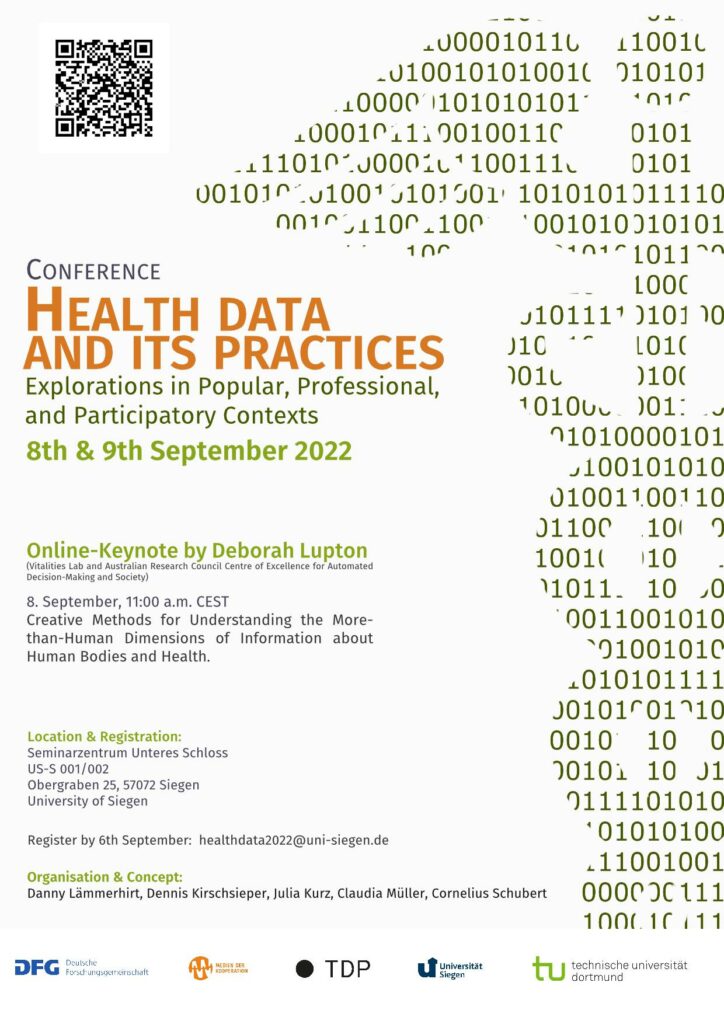
Conference Location:
Seminarzentrum Unteres Schloss
US-S 001/002
Obergraben 25
57072 Siegen
| Dinner Wednesday: | Dinner Thursday: |
| Brasserie | Zur Hammerhütte |
|
Unteres Schloß 1 57072 Siegen |
Kirchweg 7 57072 Siegen |
Register by 6th September: healthdata2022@uni-siegen.de
Schedule Long Version (including Abstracts)
Thursday, 8th September
10:30 Welcome and Introduction
11:00 Keynote: Deborah Lupton (Sydney) via Zoom
Creative Methods for Understanding the More-than-Human Dimensions of Information about Human Bodies and Health
Deborah Lupton, Vitalities Lab and Australian Research Council Centre of Excellence for Automated Decision-Making and Society, UNSW Sydney, Australia
In this presentation, I discuss how more-than-human theory can be brought together with creative methods drawing on the arts and design to surface the ways in which human bodies and health states are entangled not only with digital media and devices but also with aspects of the non-digital world. I use examples from my research teams’ projects at the Vitalities Lab and the ARC Centre of Excellence for Automated Decision-Making and Society to illustrate how we have used these methods and the insights generated concerning health information. We use the term ‘lively data’ to describe the information and marks left by humans and other living things as they move, grow, age, die and decay, constantly changing form and entering into new more-than-human assemblages. With these projects, we want to expand thinking about how we can learn about our bodies and health states by developing strong links between the materialities of our fleshy bodies and those of other living things. The methods with which we are working attempt to stimulate recognition of people’s personal data as human remains and to make the connection between nonhumans, humans and more-than-human vitalities, interconnected relationships and distributed wellbeing.
12:30 Lunch
14:00 – 15:30 Caring, Health, and Digital Technologies
Galia Assadi (Nürnberg): Trust in the Powers of Ethical Judgment. Reflections on the Ethical Value and Implications of Participatory Contexts
Ethical evaluation of digital health technologies can tread different paths. Most evaluations can be grouped in one of the following approaches: 1.) Extern ethical evaluation, mainly produced by studied ethicists and grounded on the traditions of academic discipline like e.g. philosophy or theology. 2) Accompanying research (connected to projects in the realm of technology research and development) regarding ethical, legal and social aspects (ELSA), primarily conducted by professional researchers who take part in the development processes. 3) Participatory approaches in IT development, including researchers from different areas of expertise as well as laypersons representing the targeted user group. Even though, from an ethical perspective, every approach is equivalent, they result in different outcomes and are based on a different understanding of ethics. Whereas approach 1and 2 are already well established, e.g. in the area of publicly founded technology research and development, approach 3 actually is relatively new and rarely tested. This may have its origin in the challenges connected to participatory research as well as in a deficit regarding methodical expertise. The presentations aims at demonstrating the ethical foundation as well as the potential of this approach, highlighting its ethical relevance for a pluralistic society and its fruitful implications for design and implementation of digital health technologies.
Christophe Kunze (Furtwangen): The Complexity of Cooperative Care and Health Data practices – Explorations of IT-supported Collaboration in (Tele-)care
This contribution presents explorations of health data and its practices in collaborative caregiving. It is drawing on observations and experiences in different contexts such as the coordination and collaboration of formal and informal elderly care [1], digital neighborhood development [2] and the implementation of video telecare in home-based palliative care for children [3]. While these application examples differ considerably in terms of medical challenges and actors involved, they nevertheless share many similar characteristics. As collaborative care work, they are characterized by a high proportion of interaction work. Subjective assessments, experiences as well as tacit and implicit knowledge play an important role, but are typically only partially visible in health and care data in IT systems. The inherent categorization and standardization in IT systems can only reflect diversity and complexity of caregiving contexts to a limited extent. In such collaborative care structures, the boundaries of formal and informal caregiving roles are blurring. The same is true for popular and professional health data. Participatory health data is a result of co-production, for instance in video telecare when patient’s relatives are controlling the camera work instructed by caregivers. Due to the highly dynamic nature of the digital transformation, the handling of such participatory data is less established and standardized than in formal, professional application contexts. The appropriation of tech therefore requires a high degree of infrastructural work, whereby actors can hardly draw on the experience of others and practices must be negotiated and reconfigured on a regular basis.
Our explorations highlight ambiguities, uncertainties and contradictory facets within participatory health data practices. For instance, video interaction in telecare is fluctuating between preserving and compromising privacy, keeping distance and staying connected, practical benefits and conflicting professional attitudes, and (de-)professionalization. The design, implementation and (non-)adoption of IT-supported collaboration tools and structures also reveals breakdowns and gaps within the health and social care system, such as missing responsibilities for essential care and case management tasks. Consequently, the design and implementation of health data systems and practices is also raising questions about the nature of (visible and invisible) care work and what constitutes good care.
References:
[1] Renyi, M., Gaugisch, P., Hunck, A., Strunck, S., Kunze, C., & Teuteberg, F. (2022). Uncovering the
Complexity of Care Networks–Towards a Taxonomy of Collaboration Complexity in Homecare.
Computer Supported Cooperative Work (CSCW), 1-38.
[2] Renyi, M., Hegedüs, A., Schmitter, P., Berger, F., Ballmer, T. M., Maier, E., & Kunze, C. (2022). Lessons
learned: the multifaceted field of (digital) neighborhood development. The Journal of Community
Informatics, 18(1).
[3] Kunze, C., Kächele, I., Kiefer, P., Lindwedel, U. (2022): Digitalisierung in der Pflege – aktuelle
Entwicklungen, Potentiale und Herausforderungen im Kontext der Versorgung von Menschen mit komplexer Behinderung. In: Zuleger, A., Maier-Michalitsch, N. (Eds.). Pflege und Palliative Care interdisziplinär. Verlag selbstbestimmtes leben, 2022 (in press).
Sebastian Merkel (Bochum): Using Smart Speaker for Health and Social Care by Older Users. An Explorative Study
Smart speaker, like Amazon´s Echo or Apple´s HomePod, show high rates of diffusion in private households in Europe and North America since Amazon launched the first smart speaker in the USA in 2015. Against the background of commercial success of and technological advantages in speech recognition (SP) and natural language processing (NLP), there is a growing body of literature on the use of digital assistants and smart speakers in the domain of health and social. With hands-free interaction, the devices can be used as medication reminders, for symptom management, documentation, or communication between patients and nurses/doctors covering multiple medical fields like diabetes care (see e.g. Basatneh et al. 2018; Dojchinovski et al. 2019; Sadavarte and Bodanese 2019; Sezgin et al. 2020). One group of potential users of smart speakers and benefits of smart speakers for this group have already been discussed (see e.g. Farr, 2018; Ianzito, 2018; Nimrod & Edan, 2021). Features of smart speaker (‘skills’ or ‘actions’) available specifically designed for the elderly and companies like Amazon started offering specific services such as “Alexa together”, that aim at supporting older persons living independently by offering multiple features like fall detection alerts and activity responses. Advantages of the supposedly easy to use voice assistants for older individuals seem obvious: They can be operated despite visual impairments or limitations in mobility and without the need of getting accustomed to a visual user interface, which makes them easier to navigate (Nimrod & Edan, 2021). A recurring critique in the field focuses on the question of data security, be it due to the risk of wiretapping inputs or because using voice commands is considered a new form of interaction with technologies requiring knowledge about how data is processed by users (Deutscher Bundestag, 2020). However, up to date research on smart speaker use by older persons is still in its beginnings, particularly on questions of appropriation and Appropriation of tech. Against this background, the presentation will integrate results of several studies carried out: (1) A scoping review on the use of smart speakers within the domain of health and social care, (2) a review of smart speaker applications designed for older persons, and (3) domestication of smart speakers by older persons based on interview data.
15:30 – 1 6:00 Coffee Break
16:00 – 17:30 Appropriating and Implementing Health Data Practices
Anne Jordi Koppenburger (Aachen): Taking Shape – Examining Knowledge Infrastructures for Health. On the Formation of the Electronic Patient File in Germany
Over 25 years ago the term electronic patient file (EPF) found its way into the rhetoric repertoire of health politicians not only in Germany. While the term has changed its meaning since then, especially in recent years it has become a main talking point of health politicians relating to health care system improvements. In my study of the formation of the EPF, I consider several viewpoints and trace expectations of stakeholders emerging over the course of time and under changing health policies. Initial results of interviews and documentary analysis suggest not only an interplay of different logics from different levels of the healthcare system. Moreover, the EPF can be understood as an infrastructuring endeavor that takes shape according to values inherent to the model of the health insurance system on the one hand. On the other hand, the form taken at each point of time constrains the realization of alternative and future options.
In my presentation I shall delineate the observed sociotechnical enterprise as a basic (data) preparatory work in the health care system.
Conceptualizing the electronic patient file as a boundary infrastructure (Neuman/Star 1996) allows for the consideration of different stakeholders who are directly and/or indirectly involved in the development of the basic digital infrastructure, its hard- and software and its manifold applications. From here, demanding social processes, e.g. the deliberation of (technologically-)promoted values and the negotiation of jurisdictions come into view. However, in contrast to technical artifacts, infrastructures have no clear cut life-cycles; they are conceived as timely and spaciously far-reaching (Bowker 2015). Associated herewith are methodological challenges to observe, analyze and theorize digital infrastructures not only in the health care
sector. Seen as a mode of social practice, infrastructuring and its prevalence calls for methodological innovations and new perspectives of the social studies of science and technology. Using the example of the electronic patient file, I will discuss these research related issues.
Enrico Maria Piras (Verona): Quantifying, Tracking, Analyzing. Disputed Bodies in Datafied Chronic Care Management
Datafication of the human body, the representation of vital signs and activity through figures, is not new in itself. While measuring has been a concern for medical science since its inception (Shryock, 1961), contemporary healthcare provision also heavily relies on data for administrative or procedural aspects. Representing physiological process through data serves the purpose to disentangle a single function from the messiness of the body, constantly scrutinize and correct its malfunctioning if necessary. Datafication holds the promise to unpack and make intelligible the biology of the body paving the way to streamlining the adjustment, hacking and improvement of its inner mechanisms. Data work, “the human activity related to creating, collecting, managing, curating, analyzing, interpreting, and communicating data” (Bossen et al., 2019) is so intertwined with medical practice to the point of having become indistinguishable from it and such activities have significantly contributed to change professions and reshape healthcare organizations and practices.
More recently creating, harvesting, and interpreting data have become part of the curriculum of patients and caregivers too. The emphasis on empowerment and self-management in chronic care has led to patient education requiring competences in represent their condition through measuring and making sense of data, leading to several different forms of health data tracking (Lupton, 2014). Moreover, the availability of personal monitoring devices ended the monopoly of the clinic as the locus of body data production and has paved the way to forms of health data analysis performed by patients, leading to forms of practical patient knowledge which may differ from medical knowledge (Pols, 2014).
Besides measures, personal health technologies often offer decision support systems built by manufacturers basing on the analysis of big data gathered through the devices. Proprietary algorithms, whose inner functioning is not disclosed, have thus entered the landscape of health decision making as a third legitimate interpreter of health data together with healthcare professionals and patients.
While datafication of the body has opened up opportunities for diagnosis and therapy it has also contributed to turn bodies into disputed terrains of intervention. Diabetes type 1 has a longstanding tradition as a forerunner of future trends in health care and it will provide the case to illustrate the how personal health technologies, datafication, and automated interpretation have given rise to grey areas in which it’s not clear whose interpretation is more relevant.
Focusing on three grey areas (type 1 diabetes management during pregnancy, in remote monitoring, and the self-management practices performed within the school premises) the chapter will describe and discuss how datafication technologies can be subject to multiple forms of appropriation where responsibilities are attributed and negotiated, new configurations of care are built, boundaries are created and contested.
References:
Bossen, C., Pine, K. H., Cabitza, F., Ellingsen, G., & Piras, E. M. (2019). Data work in healthcare: An Introduction. Health Informatics Journal, 25(3) 465–474
Lupton, D. (2014b). Self-tracking modes: Reflexive self-monitoring and data practices. Available at SSRN: http://dx.doi.org/10.2139/ssrn.2483549
Pols, J. (2014). Knowing patients: turning patient knowledge into science. Science, Technology, & Human Values, 39(1), 73-97.
Shryock, R. H. (1961). The history of quantification in medical science. Isis, 52(2), 215-237.
Benjamin Marent (Sussex): Digital Health: A Sociomaterial Framework
The notion of digital health often remains an empty signifier, employed strategically for a vast array of demands to attract investments and legitimise reforms. Rather scarce are attempts to develop digital health towards an analytic notion that provides avenues either for understanding and/or for governing such ongoing transformations in healthcare. This presentation elaborates a sociomaterial framework for governing digital health innovation. It first outlines a sociomaterial approach to understanding digital health, showing how digitalisation affords practices of health and medicine to handle the combined and interrelated challenges of increases in quantification (data-intensive medicine), varieties of connectivity (telemedicine), and unprecedented modes of instantaneous calculation (algorithmic medicine). This enables an engagement with questions about what forms of knowledge, relationships and control are produced through certain manifestations of digital health. The presentation then sets out, in detail, an innovative digital health governance framework that can guide explorations and negotiations into the type of care we want to achieve through digital transformation. The framework embeds Karen Barad’s concept of agential cuts suggesting that responsible cuts towards the materialisation of digital health require participatory efforts that recognise the affordances and the generativity of technology developments. Such governance strategies can lay the foundations to reorient and sensitise innovation and care processes in order to create new possibilities and value-centric approaches for promoting health in digital societies as opposed to promoting digital health per se.
KEYWORDS: digital health futures, sociomaterial governance, agential realism
19:00 Conference Dinner
Zur Hammerhütte
Kirchweg 79
57072 Siegen
Friday, 09th September
09:00 – 10:00 Clinical Health Data Practices I
Susanne Brucksch (Tokyo): Health Data, Medical Devices and Development Practices Among Clinical Engineers in Japan
Health data are nowadays mediated by machines and digital technology. They are the source for medical knowledge and health practices in professional and popular contexts alike. The scholarship draws wide attention to the generation and processing of such information and insufficiencies responding to user needs. The focus lies predominantly on medical professionals, nurses and care givers as well as patients and/or care recipients and their families. Less light is shed on the role of medical technicians and engineers who are designing, producing and maintaining devices mediating health data. In Japan, the number of technicians employed in hospitals seems to have increased two- to threefold over last 30 years with the intrusion of high-technology into clinical workplaces. This remarkable change leads to the question which role do clinical technicians and engineers play in providing and maintaining the data-related technology and infrastructure in hospitals. Moreover, how far do they rely on health data and which data practices can be observed in the making and application of medical technology. This paper presents data from an interview study conducted in Jan 2020 and Nov-Dec 2021 in various hospitals in Japan. The preliminary findings suggest that clinical technicians experience a markedly increase of their professional status in hospital hierarchies. However, they also face increasing difficulties to keep up with the employment and maintenance of highly complex devices provided by medtech companies and abroad. If this would not be enough, clinical engineers and technicians are expected to be involved in medtech partnerships to support local industries and to secure future markets for a struggling (local) economy. Special matching and exchange programs have been established to enable information flow and participatory development but came under further pressure during the pandemic resulting in limited excess to clinical sites, increased need for exchange and a switch to digital matching formats.
Susanne Brucksch is associate professor at Teikyo University in Tokyo, Japan. She was senior researcher at Free University Berlin and principal researcher at the German Institute for Japanese Studies (DIJ) in Tokyo before as well as visiting scholar at Waseda University in 2016 and the Max Planck Institute (MPI) for Innovation and Competition in 2019. Brucksch has been serving as chair of the advisory board of DWIH Tokyo (German Centre for Science and Innovation) 2019-2021 and as board member of VSJF (German Association for Social Science Research on Japan) since 2016. Her research focuses on innovation and research collaboration regarding medical devices in Japan. Her recent publications comprise the anthology „Humans and Devices in Medical Contexts. Case Studies from Japan“ (2021), edited with Kaori Sasaki, Palgrave Macmillan (https://link.springer.com/book/10.1007/978-981-33-6280-2).
Stefanie Büchner, Justus Rahn (Hannover): “Palliative” Modes – Reconfigurations of Data Practices in Intensive Care
Die Ethnographie hat interessante Einblicke in den Wechsel des Modus im Umgang mit Daten angesichts von (meist kurzen) Sterbeprozessen auf der Intensivstation gegeben, die wir gerne vorstellen und diskutieren würden. Der Titel „Palliativmodus“ greift eine Semantik des Feldes auf, nämlich die Bezeichnung für eine neue Möglichkeit, über eine spezifische Einstellung der Monitoringsysteme die Sichtbarkeit und audiovisuelle Präsentation von Gesundheitsdaten „am Bett“ zu verändern. Wir möchten uns diesem Wechsel, der natürlich weit mehr meint als die Änderung der technischen Voreinstellung, genauer widmen und damit einen Beitrag zur Datafizierung und Sterben leisten, der vielleicht auch im Anschluss an Glaser und Strauss für die Diskussion von „health data“ interessant ist.
10:00 – 10:15 Break
10:15 – 11:15 Clinical Health Data Practices II
Kevin Wiggert (Berlin): Systems of AI-assisted Clinical Decision Support. On Attempts at Data-based „Calculation“ of Disease States in Intensive Care Medicine
Today, medical routine in intensive care units is exceedingly sociotechnical (Schubert 2011). Health professionals need to interpret the signs shown by the devices and do “balancing work” (Mort et al. 2005). Arising uncertainties are counterbalanced by the individual routine and experience of the clinician. In recent years, systems of AI-assisted clinical decision support (CDSSs) have been designed to remedy this situation (Sloane & Silva 2020). In addition to artificially intelligent calculation, CDSSs use large amounts of data. These are usually very different types of data, containing personal data, medical measurements, but also scores that have become an established part of the medical field in question. While developing such a system, it often happens that new variables are included (first on a test basis) that were not previously common practice in the relevant medical community. At the same time, other “data” sources are left out. This especially counts for the various approaches and routines of clinicians to examine a patient’s body, which constitutes a significant part of their experience base and expertise. The amount of data variables used, the diversity of the data types, as well as the substitution with and addition of new data variables that comes with the development and implementation of CDSSs makes it potentially difficult – if not impossible – to understand the procedural processes of its reasoning and how and why it came to certain conclusions. This is also one reason why their actual use is still scarce (Winter & Carusi 2022). I will use interview data with developers and clinicians from two empirical examples of the development and testing of a CDSS for the early prediction of patients’ health status in intensive care situations (one case is about monitoring the health condition in pediatric care, the other case about observing health statuses regarding potential future decompensation of patients), which I conducted in 2021 and 2022. In both cases a CDSS correlates multiple data points to potentially medically relevant results, which firstly, are difficult to validate by the treating clinicians; secondly, they are changing the temporal structure of medical examination, for example, when the predictive calculations about a patients’ health condition shown by a CDSS exceed the temporal horizon of the treating clinician; and thirdly, arise in a socio-technical context, which is often characterized by a high stress level and time pressure, which therefore makes fast decision-making necessary. In my talk I want to show how this threefold combination potentially changes medical decision-making and challenges the multiple practices of medical examination (Mol 2002).
Bibliography:
Mol, A. (2002): The Body Multiple. Ontology in Medical Practice. Durham, London: Duke University Press.
Mort, M., Goodwin, D., Smith, A. F., & Pope, C. (2005): Safe asleep? Human–machine relations in medical practice. Social Science & Medicine, 61(9), 2027-2037.
Schubert, C. (2011): Die Technik operiert mit. Zur Mikroanalyse medizinischer Arbeit. In: Zeitschrift für Soziologie, 40(4). Stuttgart, pp. 174-190.
Sloane, E. B.; Silva, R. J. (2020): Artificial intelligence in medical devices and clinical decision support systems. In: E. Iadanza (ed.): Clinical engineering handbook. Second edition. London, San Diego, CA: Academic Press, pp. 556-568.
Winter, P. D.; Carusi, A. (2022): (De)troubling transparency: artificial intelligence (AI) for clinical applications. In: Medical humanities. DOI: 10.1136/medhum-2021-012318.
Torsten Risør (Tromsø): Trailblazing, Jamsession and the Root Metaphors of Data Use in Clinical Practice
I plan to talk about five different underlying metaphors in clinical decision making – two that are mostly used by clinicians and two that are mostly used by administrators and policy makers, and finally a fifth that may explain something about why we clinicians find it difficult to adress social inequalities of health.
My empirical starting point will be an everyday clinical encounter from general practice, fairly simple in medical terms but with an inherent social complexity and useful to illustrate how the different underlying metaphors may impact decision-making.
11:15 – 11:45 Break
11:45 – 12:45 Health Data Infrastructures and Data Flows
Marine Al Dahdah (Paris) via Zoom: Digital Health for All Constructing a Data-Driven Welfare State in the Global South
Mobile phones, and more generally digital infrastructures, are now being promoted as a fundamental element in the response to health needs in wealthy countries, but also increasingly in the Global South where digitalisation is placed at the centre of „universal health coverage initiatives“. Frequently, these technical public-private partnerships determine the provision of state welfare and differentiate access to health resources through digital infrastructures. Focusing on two such initiatives in Kenya and India, this communication investigates the partnerships between government and private digital operators as well as the ability of patients to manage their health needs digitally. While these programmes promise health coverage for all, their technical infrastructures complicate access to health services, revealing new patterns of exclusion. Indeed, inclusion, exclusion and their differentiation are determined not only through public state policies but also through digitally constructed criteria. This communication also addresses questions around health data usage and ownership. Like Airbnb which does not own hotels, digital health platforms do not own physical healthcare infrastructures themselves, but they have ownership over a secondary infrastructure in the form of digitised health information. Indeed, such programmes lead to the commodification of healthcare and the weakening of public health infrastructures by diverting public funds to private digital ventures and transferring health data ownership to private companies.
François van Schalkwyk (Stellenbosch): Hyperlocal Data Flows: A Synthesis of Findings from Three African Countries
The use of health data at the local level – that level of governance and delivery of public services closest to communities – is seen as playing an important role in the evidence-based decision-making and consequently, instrumental in local development. Investments in improving the quality and use of health data in developing countries is characterized by stalled attempts to devolving governance, the interventions of multiple donors often targeted at specific diseases (e.g. HIV/Aids, malaria, TB), and a belief in the transformative potential of digital infrastructure and solutions in a context of historical underinvestment in key public services such education and healthcare. Against this background, three studies were commissioned to investigate the flow of health data between the hyperlocal and national levels of governance in Cote d’Ivoire, Lesotho and Tanzania. The purpose was to identify flows and blockages so as to design interventions that could improve data use by communities in these three countries. This paper synthesizes the findings from these three studies. It presents two general findings. First, it reveals the complexities of studying health data flows in national systems and suggests how future research could approach the study of health data flows. Second, it synthesizes the general characteristics of the flow of health data to and from the hyperlocal level in the three African countries.
12:45 – 13:00 Closing Discussion
What Makes Health Data Popular, Professional and Participatory and Why Does it Matter?
13:00 – 14:00 Lunch und Farewell
